Insomnia in Women: How Hormonal Changes Affect Sleep
Sleep is an integral part of general health and well-being. There are, however instances in which the sleep of many women is interrupted; primarily insomnia, at various stages of their lives. According to studies, women suffer from more cases of insomnia as compared to men. Hormonal changes are one of the main reasons for that; hormonal changes affect the quality of sleep but also overall mood, energy levels, and mental health.
Estrogen and progesterone are some of the hormones that have a critical role in regulating sleep patterns. The changes in the levels of these hormones, caused by the menstrual cycle, pregnancy, postpartum changes, or menopause, can disrupt sleep. PMS and perimenopause also add to sleep difficulties.
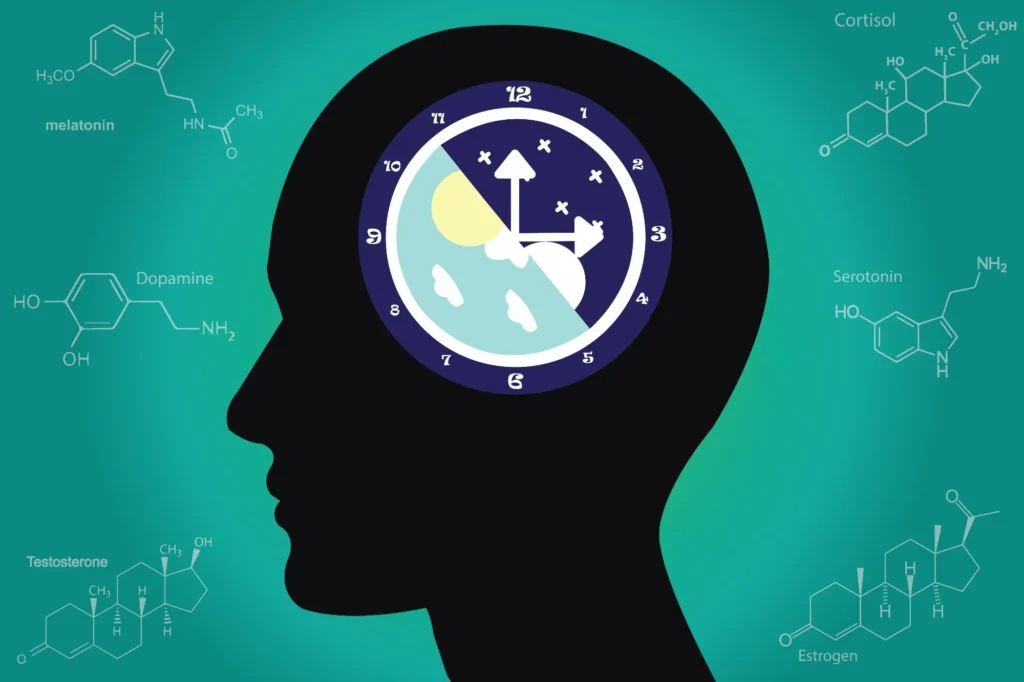
The interaction between hormones and sleep is very complex; it involves a combination of body circadian rhythm, temperature regulation, and the response to stress. Knowing such interactions may better enable women to make informed decisions regarding their sleep health. Indeed, addressing these hormonal influences by applying practical changes in lifestyle would enhance sleep quality and general well-being among women.
In this blog, we will delve into the many ways hormonal changes can affect sleep across the different life stages and learn several practical strategies to mitigate the effects.
The Link Between Hormones and Sleep
Hormones are chemical messengers that regulate various bodily functions, including sleep. Two primary female hormones, estrogen and progesterone, have significant effects on sleep quality. These hormones influence the sleep-wake cycle, mood regulation, and body temperature, all of which play crucial roles in restful sleep. When their levels fluctuate, sleep disturbances can occur, leading to insomnia, night sweats, and frequent awakenings.
1. Puberty and Sleep Disturbances
The onset of puberty brings about major hormonal changes, wherein levels of estrogen and progesterone increase. These may cause an alteration in the circadian rhythm, thus delaying the sleep-onset time. Many adolescents end up staying up late and have difficulty waking up on time. The hormonal changes that occur due to puberty also increase the likelihood of premenstrual syndrome, which characteristically includes insomnia among other symptoms. In addition, mood swings associated with puberty can also lead to anxiety, which can make it difficult to fall asleep and stay asleep.
2. Menstrual Cycle and Sleep
Hormonal changes often affect women during different phases of their menstrual cycle and lead to sleep problems. Estrogen increases in the follicular phase, and this might increase the likelihood of better sleep. In the luteal phase, the level of progesterone increases, which leads to higher body temperature, night sweats, and restless sleep. During the premenstrual period, women may suffer from bloating, cramps, anxiety, and mood swings, all of which can affect their ability to sleep.
3. Pregnancy and Sleep Disturbances
Pregnancy again imposes another degree of hormonal and physiological disturbances. The increase in the level of progesterone during the first trimester leads to sleepiness in the day-time and broken sleep at night-time. However, other physical discomforts, nausea, and urination enhance sleep disturbance. Most of the women also develop RLS and sleep apnea during pregnancy, which complicates restful sleep.
4. Postnatals Sleep Disturbances
Right after delivery, the hormone levels decline drastically, affecting sleep quality. The rapid decrease in estrogen and progesterone causes mood swings, anxiety, and postpartum depression that can lead to insomnia. Sleep is also interrupted by newborn care because of the frequent nighttime feeding and irregular sleeping patterns, leaving new mothers unrefreshed. Melatonin levels may also be affected by frequent nighttime awakenings, making it hard to get into a rhythm of sleep.
5. Perimenopause and Menopause
Perimenopause, the transitional phase before menopause, and menopause itself bring dramatic hormonal changes that can severely impact sleep. As estrogen and progesterone levels decline, many women find it difficult to fall asleep and stay asleep. Hot flashes and night sweats often cause frequent awakenings, making it hard to get restful sleep. Additionally, the risk of developing sleep apnea and restless leg syndrome increases, further exacerbating sleep issues. Mood disorders including anxiety and depression also increase around menopause; this can trigger chronic insomnia as well.
How Benzodiazepines help managing insomnia in women?
Benzodiazepines are a class of medications commonly prescribed for anxiety, muscle relaxation, and sleep disorders, including insomnia. They work by enhancing the activity of gamma-aminobutyric acid (GABA), a neurotransmitter that slows brain activity, promoting relaxation and sleep. For women, insomnia can be triggered by various factors, including hormonal fluctuations, stress, anxiety, and underlying medical conditions. Benzodiazepines can be an effective short-term solution to help regulate sleep patterns.
How Benzodiazepines Work for Insomnia
Benzodiazepines, such as diazepam, lorazepam, and temazepam, bind to GABA receptors in the brain, increasing the calming effects of GABA. This results in:
- Shortened Sleep Onset: Helps individuals fall asleep faster.
- Increased Sleep Duration: Reduces nighttime awakenings and improves overall sleep quality.
- Reduced Anxiety and Muscle Tension: Beneficial for those whose insomnia is linked to stress or muscle tightness.
Why Women May Need Benzodiazepines for Insomnia
Women often experience sleep disturbances due to hormonal changes throughout their lives, including:
- Menstrual Cycle – Fluctuations in estrogen and progesterone can lead to difficulty falling asleep or staying asleep.
- Pregnancy – Increased stress, physical discomfort, and hormonal changes may cause sleep disturbances.
- Perimenopause and Menopause – Decreased estrogen and progesterone levels can lead to hot flashes, night sweats, and insomnia.
- Postpartum Period – Sleep deprivation and anxiety after childbirth can contribute to insomnia.
In these cases, benzodiazepines may be prescribed temporarily to help women regain normal sleep patterns, particularly if other treatments, such as cognitive behavioral therapy for insomnia (CBT-I) or lifestyle changes, are ineffective.

Improve Sleep While Changing Hormones
Hormonal changes, whether due to menopause, pregnancy, or monthly cycles, can disrupt sleep by affecting melatonin production, body temperature, and stress levels. To improve sleep, maintain a consistent bedtime routine, limit caffeine and screen exposure before bed, and practice relaxation techniques like deep breathing or meditation. Keeping your bedroom cool and dark, along with incorporating light exercise and a balanced diet, can also help regulate hormones and promote restful sleep. If sleep disturbances persist, consider consulting a healthcare professional for personalized solutions. However, Hormonal changes can not be helped but their interference in sleep could be managed.
1. Have a Scheduled Sleep Pattern
Bedtime and waking up in the morning always help regulate a body’s clock.
2. Keep you bedroom quiet
Keeping the bedroom cool, dark, and quiet can encourage sleep and reduce disruptions due to hormonal fluctuations.
3. Reduce Caffeine and Alcohol Intake
Both of these substances can disrupt the body’s ability to fall asleep and stay asleep, especially during hormonal shifts.
4. Exercise Regularly
Physical activity helps regulate hormones and improves sleep quality. However, intense exercise before bedtime can stimulate the body and make it difficult to relax.
5. Relaxation Techniques
Yoga, meditation, and deep breathing can help decrease stress and make it easier to fall asleep.
6. Manage Hot Flashes
Using breathable fabrics, cooling pillows, and fans may help minimize discomfort at night.
7. Consider Professional Help
If sleep disturbances persist, consulting a healthcare provider for potential hormone therapy or other sleep interventions may be necessary.

Conclusion
Hormonal changes during a woman’s life course can greatly contribute to her poor sleep and insomnia. Changes in life usually begin with physiological changes, which need to be confronted actively by women.
While it might be very frustrating to have sleep disruptions caused by hormonal changes, such issues are not unavoidable. Even slight lifestyle, sleep hygiene, and stress management can create a better quality of sleep. Self-care and the importance of good sleep should be prioritized to help women navigate these challenges more effectively. If symptoms persist, medical advice is sought to ensure the right treatment approach is taken. Ultimately, a well-rested body and mind contribute to better overall health and a higher quality of life.
1 thought on “Insomnia in Women: How Hormonal Changes Affect Sleep”
Comments are closed.







You’ve hit the nail on the head with this one! Cheers.